Mark Reed, DPM
DABFAS FAPWCA

714-528-3668
Neuropathy Cause & Treatment
Dr. Mark Reed began using nitroglycerin patches in 1989 as a Resident at UCSF / VASMSF to first treat diabetic ulcers to stimulate small vascular arteriole blood flow that resulted in increased ulcer healing rates. In using nitroglycerin to treat Wound Care patients, these patients with peripheral and autonomic neuropathy began reporting their peripheral and autonomic neuropathy symptoms were being reversed. Over the last 30 years, Dr. Reed has developed a nitroglycerin patch protocol that has reversed more than 3000 patients with peripheral and autonomic neuropathy and prevented countless diabetic ulcers from occurring.
For Diabetic Wound Care Information,
click here.
For Diabetic Foot Care Information, click here.
For Diabetic Nutritional Guideline Information, click here.
For Diabetic Foot Infection Information, click here.
For Diabetic Charcot Foot Deformity Information, click here.
For Peripheral Arterial Disease Information, click here.
DIABETIC NEUROPATHY (DNP) CHALLENGES AND NITROGLYCERIN
One of the most significant pathophysiology complications of Diabetes is neuropathy pain and or numbness that to date continues to represent a therapeutic challenge. Schreiber AK, et. al., Diabetic neuropathic pain: Physiopathology and treatment. World J Diabetes. 2015 Apr 15;6(3):714-528-3668. Doi: 714-528-3668/6. i3.432. Nitroglycerin has been prescribed for over 75 years to reverse oxygen ischemia causing angina pectoris by vasodilation of the microcirculation involving the arterioles. Nitroglycerin has been used for more than 33 years by Dr. Mark Reed to increase the microcirculation of the arterioles in the lower extremity in using nitroglycerin patches for 12 hours during the day that has the same effect on reversing the same angina symptoms in the feet in reducing or eliminating radiating burning pain in the feet. These findings were reported with significant reduction in pain in using transdermal nitroglycerin. Taheri A, Farbood et.al., “The effect of transdermal nitroglycerin on pain control in diabetic patients with peripheral neuropathy.” J Diabetes Metab Disord. 2015 Dec 1; 14:86. For wound healing, Dr. Reed has the patient place an additional patch proximal to the ulcer that increases oxygenation and white blood cell migration into the healing wound tissues.
NEUROPATHY DEFINED and TYPES
Diabetic neuropathy is a debilitating disorder that occurs in nearly 50 percent of patients with diabetes. Diabetic neuropathy in type 1 diabetes can present as a late finding after having the disease for more than five years and can be an early finding in type 2 diabetes. Diabetic and non-diabetic neuropathy are peripheral sensorimotor and autonomic. Sensorimotor peripheral neuropathy involves sensory symptoms of pain, paresthesia, numbness, paralysis, cramping, nighttime loss of balance and antalgic unstable gait. Autonomic neuropathy involves dysfunction of cardiac, genitourinary, sudomotor, endocrine and cerebral systems.
Patients may present with only one type of diabetic neuropathy or may develop combinations of neuropathies as distal symmetric polyneuropathy. Distal symmetric polyneuropathy is the most common form of diabetic neuropathy where a patient presents with numbness, tingling, and/or pain that begins in the toes and slowly spreads into the foot and up the leg. Because the symptoms are often present in the areas covered by gloves or stockings, peripheral neuropathy is often described as having a "glove and stocking" distribution of symptoms.
Autonomic neuropathy causes dysfunction of major organ systems responsible for sustaining life that we do not actively control. Autonomic cardiovascular neuropathy can involve silent cardiac ischemia, orthostatic hypotension, vasomotor instability, exercise intolerance, fatigue, heart rate arrhythmia, syncope, dizziness, lightheadedness, and balance problems. Autonomic Gastrointestinal neuropathy symptoms can involve dysphagia, gastroparesis, bladder dysfunction, bloating, nausea and vomiting, diarrhea, constipation, loss of bowel control. Autonomic Sudomotor (sweat glands) neuropathy symptoms can involve hyperhidrosis or excessive sweating, pruritus, dry skin, limb hair loss, calluses, and reddened areas. Autonomic Endocrine neuropathy symptoms can involve hypoglycemic unawareness. Autonomic Cerebral autonomic symptoms can involve sexual dysfunction, difficulty driving at night, depression, anxiety, sleep disorders, loss of food taste, decreased speech frequency and cognitive memory loss.
DIABETIC PERIPHERAL & AUTONOMIC NEUROPATHY CAUSES
Diabetic neuropathy is specific to the neuropathy caused from loss of oxygen to tissues and organs due to small vessel arterioles caused by excessive blood glucose. Diabetic neuropathy can affect any part of the nervous system and not just the skin of the feet as commonly believed. Diabetic neuropathy should be suspected in all patients with type 2 diabetes and in patients who have had type 1 diabetes for more than five years. In some instances, patients with diabetic neuropathy have few complaints, but their physical examination reveals mild to severe sensory loss to their forefoot and balance instability. Idiopathic (unknown) neuropathy has been found to precede the onset of type 2 diabetes or to occur as an early finding in diabetes.
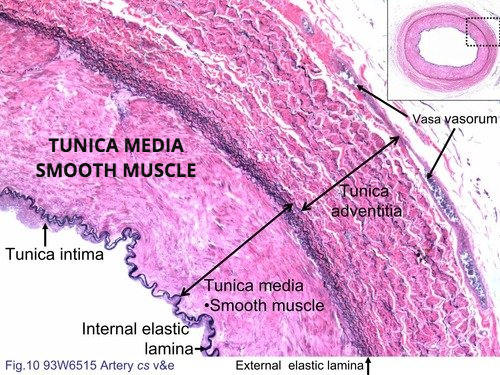
From an arterial standpoint, Diabetic peripheral neuropathy results from the somatosensory nerves in the skin becoming damaged from chronic high blood sugar that affects the small arteriole tunica medica smooth muscle. The arteriole tunica medica smooth muscles normally contract and relax in response to temperature and are the only muscle that can absorb glucose without insulin. When high blood glucose is occurring, the tunica medica smooth muscle absorbs glucose and then water follows to swell the wall of the arterioles and narrow the blood flow to the capillary that releases oxygen to the tissue.
Diabetes also causes Leukocyte dysmotility where the white blood cells swell and cannot move out of the artery to migrate to the location of an infection. In addition, dysmotility (not being able to migrate out of the arterial wall) occurs to fibroblasts (scar forming white cells) and osteoblasts (bone forming white cells). Thus, Diabetic patients who have uncontrolled blood glucose that results in osmotic swelling develop peripheral and autonomic neuropathy but also are immunocompromised to fight an infection as well as take a lot longer to heal soft-tissue and bone injuries.
When peripheral neuropathy becomes dangerous is when the nerves to the foot stop functioning and pain cannot be felt. This is known medically as the loss of The Protective Threshold of Pain. Clinically this is when a patient can no longer feel a Semmes-Weinstein monofilament (SWM) probe to their forefoot. The danger in losing the protective threshold of pain is the patient will get ulcers due to placing significant additional pressure on the forefoot to ambulate causing further loss of oxygen to the tissues.
Peripheral neuropathy will develop in about 60% to 70% of all people with diabetes as a national average. However, diabetic patients who control their blood glucose levels can reverse their type 2 diabetes and go into Diabetic Remission. Diabetic Remission is where the patient has achieved a Hemoglobin AIC level below 6 that usually is a combination of strict medication compliance and weight loss using intermittent fasting and or small portion dieting. If a Diabetic patient maintains their Hemoglobin AIC below 6, from a medical standpoint, they will stop a multitude of physiological processes that damage their tissues. Unfortunately, many patients intentionally skyrocket their glucose in eating known high glucose deserts and other foods like pastas and then inject additional insulin thinking there is no harm. Such hope is not lived long due to the irreversible medical consequences of giving yourself additionally insulin shots after skyrocketing your glucose that results in non-healing ulcers, dialysis, blindness and usually lower extremity amputations.
Non-DAIBETIC PERIPHERAL & AUTONOMIC NEUROPATHY CAUSES
Peripheral and Autonomic Neuropathy can be caused by many other diseases and conditions as follows: Alcoholism, kidney failure, vitamin deficiency (particularly B12 and folate), shingles (post herpetic neuralgia), Fibromyalgia, Complex Regional Pain Syndrome, Autoimmune diseases (Lupus, Rheumatoid arthritis or Guillain-Barre syndrome), AIDS, syphilis, and inherited disorders (amyloid polyneuropathy or Charcot-Marie-Tooth disease. In addition, neuropathy can be caused from exposure to toxins (heavy metals, gold compounds, lead, arsenic, mercury, and organophosphate pesticides), cancer therapy drugs (Vincristine, Oncovin and Vincasar), and antibiotics (metronidazole, Flagyl and Isoniazid). Rare causes of neuropathies include neurofibromatosis, congenital neuropathies (Fabry disease, Tangier disease, hereditary sensory autonomic neuropathy, and hereditary amyloidosis) and anti-cholesterol statin medications. In the extremities, peripheral nerve entrapments can cause peripheral neuropathy due to excessive pressure including tarsal tunnel syndrome in the ankle and carpal tunnel syndrome in the hand. Besides these many causes, many patients have no known cause and are diagnosed with idiopathic peripheral neuropathy.
WHAT ARE THE SYMPTOMS OF PERIPHERAL NEUROPATHY
Peripheral neuropathy is a disorder of nerve(s) apart from the brain and spinal cord. Patients with peripheral neuropathy may have tingling, numbness, unusual sensations, weakness, or burning pain in the affected area. Oftentimes, the symptoms are symmetrical and involve both hands and feet.
Autonomic Neuropathy can present with many differing symptoms depending on the nerve involved, including numbness, pain of different types, weakness, or loss of balance. Because the autonomic nerves control bodily functions that we do not consciously think of, such as heart rate, digestion, and emptying of the bowel and bladder, autonomic neuropathy manifests with symptoms affecting the loss of control of these functions. Symptoms may include problems with blood pressure, voiding, passage of stools (diarrhea, or constipation), heart rate, or sweating. Cranial neuropathy is similar to peripheral neuropathy, except that the cranial nerves are involved. Any of the cranial nerves can be involved. One of the more common causes of cranial neuropathy called ischemic optic neuropathy is loss of blood flow from the optic artery to the optic nerve.
Specific nerves can be involved in neuropathy. When a specific nerve is involved, the symptoms are limited to the distribution of that nerve. The most commonly involved peripheral nerve is the posterior tibial nerve in the ankle called tarsal tunnel syndrome or the median nerve at the wrist called carpal tunnel syndrome. Essentially any peripheral nerve can become entrapped and cause the signs and symptoms of neuropathy. Surgical excision of nerve tumors or neuromas can result in neuropathy when the cut nerve cannot reconnect and an amputation neuroma resulted that present with constant, burning, radiating, tingling type pain. Trauma can also affect nerves that are susceptible to traumatic injury such as the ulnar nerve is commonly entrapped at the elbow, the peroneal nerve to the outer part of the knee, the pudendal nerve in the pelvis and lateral femoral cutaneous nerve at the waist.
WHAT TESTS DIAGNOSE PERIPHERAL NEUROPATHY?
Because peripheral neuropathy has so many causes and so many presentations, the first step to diagnosis is performing a thorough medical history and physical examination. Certain tests done during the physical exam, including vibration and Semmes-Weinstein monofilament testing, are very accurate in diagnosing certain types of peripheral neuropathy, such as peripheral neuropathy seen with diabetes. In addition, 50% of Diabetic type 2 diabetes who have neuropathy have associated large vessel peripheral vascular disease that involves narrowing or stenosis of the large leg arteries. If you have type-2 diabetes and have neuropathy, it is important to ask your doctor to evaluate your large vessels in testing your lower extremity pulses and to have the doctor order a doppler vascular lower extremity study if warranted. Early diagnosis of large vessel peripheral vascular disease and corrective vascular intervention is important to treat this limb and life-threatening medical condition before a foot ulcer and resultant infection occurs.
The Capillary Refill Time (CRT) tests the refill of blood to the skin to pressure proving there is a small vessel vascular pathology. Sensory testing of patients with diabetes is an integral part of preventing new and recurrent foot ulcers. The Semmes-Weinstein monofilament (SWM) test is used to screen for loss of protective sensation and if a positive test is noted in an examination, peripheral arterial doppler testing should be ordered to rule out peripheral vascular disease. Blood tests for exposure to toxins and electrodiagnostic studies, such as nerve conduction studies (NCS) and electromyography (EMG) are also useful. Either skin biopsies or quantitative sudomotor axon reflex testing (QSART) is used to help diagnose different types of neuropathies.
TREATING AND REVERSING PERIPHERAL NEUROPATHY!
The treatment for peripheral neuropathy first must be focused if a treatable cause can be diagnosed in assessing the medical history, clinical findings and then perform appropriate laboratory tests due to the many causes of neuropathy as discussed above. As a fundamental treatment, a patient with neuropathy should have an evaluation by their Primary Doctor to ensure their diabetes is controlled and any other major medical issues are addressed. Dr. Reed also recommends diabetic patients adopt an intermittent fasting program every day that skips breakfast to decrease the dependency on glucose and insulin and to burn fat to maintain the metabolism. Controlling diabetes will prevent the progression of neuropathy. Where local causes of neuropathy are diagnosed these are corrected such as peripheral nerve entrapments including tarsal tunnel syndrome or carpel tunnel syndrome using physical therapy, alcohol injections, and or surgery. Where systemic causes are diagnosed, these issues are also addressed.
For Diabetic and non-Diabetic peripheral and autonomic neuropathy, Dr. Mark Reed has been using nitroglycerin for 30+ years to treat peripheral and autonomic neuropathy. Nitroglycerin has a mechanism of action of vasodilatation of the Tunica Media smooth muscle of the small arterioles that increases blood flow to the capillaries responsible for oxygen release to the surrounding tissues. This arteriole vasodilatation due to the nitroglycerin reverses the oxygen tissue damage from narrowing of the arteriole lumen due to excessive glucose osmotic swelling or from unknown causes in idiopathic neuropathy.
Dr. Reed assesses the effectiveness of nitroglycerin using the Capillary Refill Time as well as the temperature of the forefoot that is abnormal in diabetic and idiopathic neuropathy. Each patient has a different sensitivity to nitroglycerin. However, for most patients who are stared on a loading dose of nitroglycerin, their ischemic pain and related paresthesia disappear within the first week of administration. As the loading dose is adjusted for each patient, a therapeutic dose based is reached based on their Capillary Refill Time (CRT) becoming normalized. Once a therapeutic dose is reached, almost all patients experience over the next three to five months skin nerve regeneration as feeling increases in the feet and their confidence in walking improves. This response is most significant in patients with normal physiology with no underlying health issues who have peripheral neuropathy from fibromyalgia or cancer chemotherapy treatments. Besides nitroglycerin causes the increase release of oxygen from the capillaries to the nerves of the skin, there is also reversal of autonomic neuropathy symptoms in providing increased capillary oxygenation to major organ systems such as the eyes, kidney and brain. Based on Dr. Reed prescribing nitroglycerin for Diabetic patients for 30+ years and observing their long-term medical benefits, Dr. Reed placed all neuropathy patients on lifetime regiments. Such a lifetime regiment combined with controlling diabetic blood glucose levels will help prevent peripheral and autonomic neuropathy to varying degrees and helps prevent foot ulcerations.
There are many medications that help a patient manage the pain or discomfort of having painful or numb feet and or autonomic neuropathy complications. However, none of these following medications actually cure the underlying small vessel oxygen damage from excessive blood glucose from diabetes. Topical application of Capsaicin, (the chemical in chili peppers gives a hot feeling) and menthol liquids and creams are available over the counter to help distract the feeling of the pain of peripheral neuropathy.
PREVENTATIVE INTERVENTION
When a patient cannot feel pressure or pain to their feet, this is known as the Loss of the Protective Threshold of Pain, that requires the patient to adopt numerous preventative interventions. These would include looking at their feet every day, restricting walking to 30 minutes with 5 minutes of rest to revitalize the skin to the bottom of the foot, protective diabetic shoes with pressure reducing insoles, never walking barefoot around the house, three-month checkups with the Doctor managing your diabetes and bimonthly visits to the Foot Specialist. In addition, if a prominent callous or purple callous is observed, the patient must not wait but make an urgent appointment with a Foot Specialist and limit weight bearing as much as possible.
EXERCISE CAN REDUCE NEUROPATHY PAIN
Low impact exercise can reduce the pain from peripheral neuropathy due to increased tissue oxygenation. If you have not exercised in some time, plan to a gradually ease into an exercise program over days and weeks. As you slowly improve you should set a goal to exercise about 30 minutes a day alternating days to allow your body to recover.
Before staring an exercise program, you should discuss your plans with your Doctor to insure there is not issues based on checking the status of your heart, eyes, kidney and feet. You should also discuss with your doctor what glucose levels you should have in testing your blood glucose before and after exercise and what you should do on a sliding scale if glucose levels go too high. In addition, it is important to have a source of glucose available during exercise such as hard candy if your glucose drops to low.
Low–impact exercises that do not place excessive pressure on the bottom of the feet are usually well-tolerated by diabetic patients. Exercises such as swimming, water aerobics, recumbent bicycle riding, rowing machine, and yoga are usually good choices. High-impact exercises may actually make peripheral neuropathy worse or cause further nerve damage due to the excessive pressure placed on the feet to balance with neuropathy.
BALANCE EXERCISES
Balance is a learned neuromuscular skill that improves with practice. Balance exercises should be performed at least once-a-day every day. On average, after six weeks of balancing every day, patients will report a marked improvement in balance control and confidence in their ability to walk. Before balancing, place yourself in front of a counter to so both hands can grab the counter if you begin to lose your balance. Balance on one foot at a time for 30 seconds and alternate for ten times. As balance improves, the duration should be increased to one minute on each foot for five times. If you cannot actually balance on one foot, then lift the heel of one foot while balancing on the other for 30 seconds.
In addition to balancing each day, standing on your tip toes should be also performed. While standing in front and holding onto a countertop, raise up on both toes and hold the position for 30 seconds. Repeat standing on the toes for five times with the goal to increase standing on your tip toes for one-minute for five times.
NEUROPATHY SCAMS
There are many scams ongoing by so called Neuropathy Experts. These Neuropathy Experts have no training or scope of practice to treat diabetic patients or any patient with neuropathy. Neuropathy treatment is covered by Medicare so there should never be a payment made for a special non-covered treatment. Typical neuropathy scams involve free dinners with high-pressure sales fear tactics with fake paid testimonials trying to con $8,000 to $12,000 from mostly elderly victims. Treatments involve heat lamps, lasers or vibrators or amazing vitamins and herbs with fake medical research.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL. This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.